Background
Multimorbidity (MM) and complexity is a pressing problem in medicine and healthcare, affecting about 30% of the adult population and a much larger proportion of hospitalized patients. However, multimorbidity and the associated problems are often inadequately dealt with in healthcare, leading to a higher morbidity and mortality, and a reduction in quality of life for both patients and their families and relationships. In addition, the lack of coordination, continuity, and comprehensiveness in patient care (ACP 2006, Advanced Medical Home), for example the increase in circuitous patient itineraries, overlaping measures and at the same time blind spots, lead to higher cost for the health care system.
This situation is resulting from specialization in education, teaching, innovation, research, and medical services with a tendency towards addressing individual diseases within specialized expert organizations. At the same time, patients in an increasingly aging society are more frequently presenting with concurrent acute and chronic health issues. Medical and social advances increase the survival rate for risk factors, potentially leading to further health challenges. Depending on the severity and complexity of various conditions, a unique combination of diseases and treatment options must be evaluated in a complex pattern to achieve the best possible outcome for patients. Medical decisions are increasingly made within the context of multimorbidity.
Yet the true complexity of MM relates to the complex interactions of several co-existing diseases in the same person (Disease-Disease Interactions, DDIs), not in the number of diseases. Managing potentially harmful and complex DDIs in multimorbid patients is a major challenge, especially at the concrete operational level, as there are only few studies and virtually no guidelines or guidance available on these very prevalent issues. Thus, there has been little awareness of these robust questions in medicine and society. DDIs can significantly impact the care and safety of multimorbid patients. Guidelines for multimorbidity are scarce, even for the most or more common forms, for example pain management in patients with hypertension (about 5% of the adult population). This leads to a reliance on clinical guidelines intended for the treatment of individual diseases which rarely cover the issues of DDIs. Moreover, there is little medical evidence available, as multimorbid patients are often excluded from clinical trials. Therefore, physicians often draw upon their extensive personal experience to navigate therapeutic dilemmas arising from conflicting, disease-specific guidelines. These decisions depend on a physician’s personal positive or negative experiences, as well as their fundamental personality traits related to risk aversion, or other characteristics such as maximizing versus satisficing.
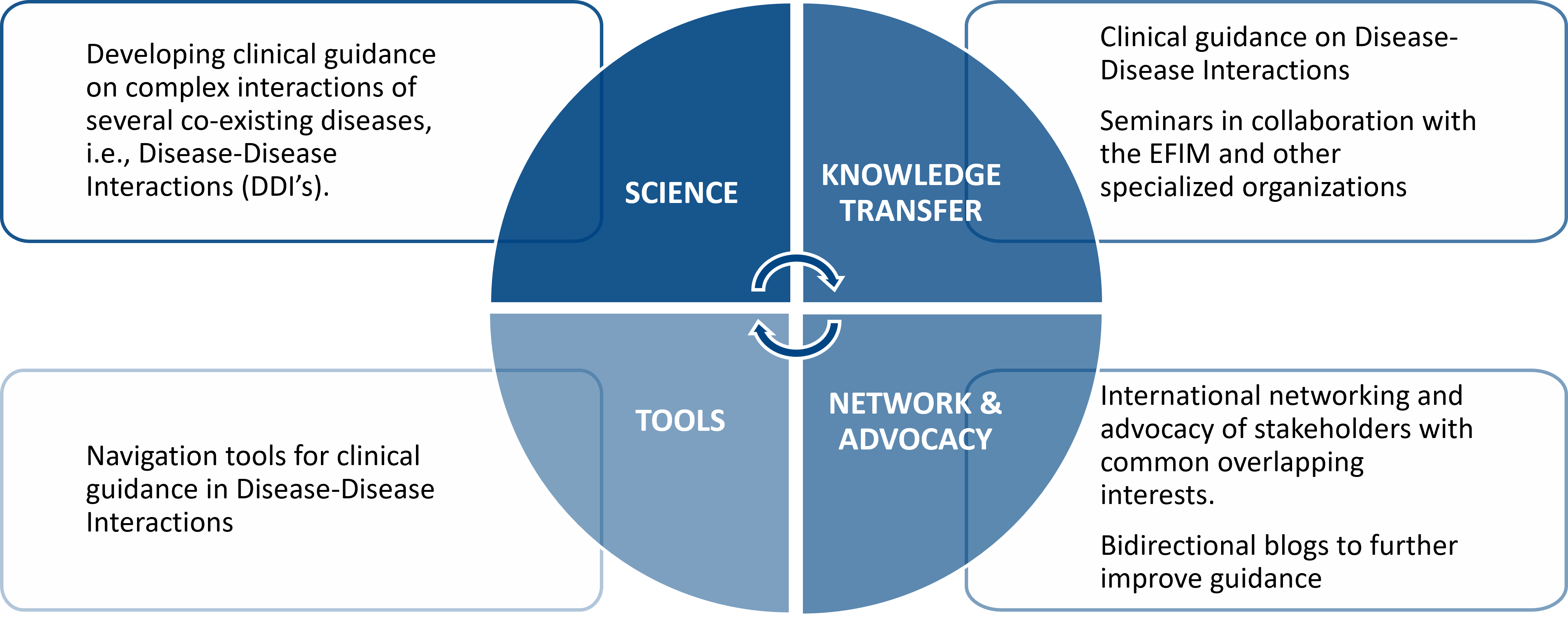
Our Approach to Multimorbidity
The projects are designed on the timeline in three consecutive and partially overlapping stages:
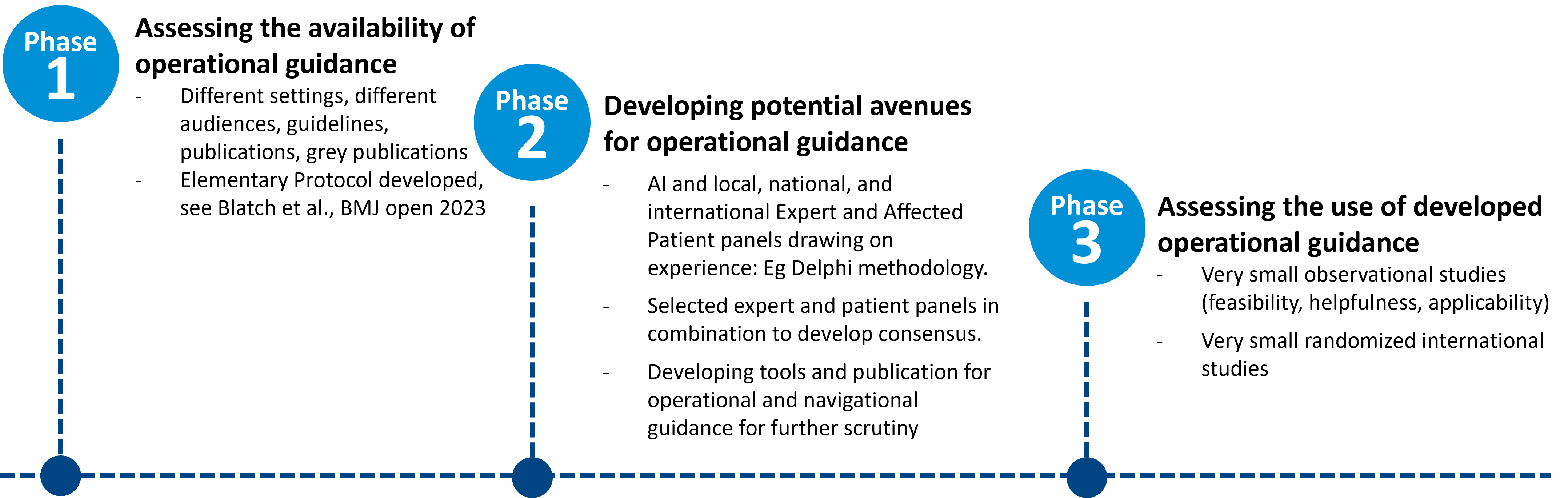
Exemplary projects were able to further explore aspects of DDI's, especially depression and other conditions such as depression and Covid-19 or comparisons between two systems with completely different settings (Zurich versus Hong Kong).
General Aims
In the long term, evidence-based medicine, experience-based medicine, psychological aspects of decision-making and patient management by physicians, and Artificial Intelligence (AI) should be integrated to help frontline clinicians with common clinical challenges concerning DDIs.
The focus of innovation activities is on physician decision dynamics, based on:
- Evidence-based physician decision-making
- Physician experience-based decision-making
- Psychological aspects of physician decision-making
- Combined description, visualization, and mapping of the corresponding complexity of decision-making, also as a basis for test sets for Hybrid AI
- Consideration of developments in society and healthcare
ICMC is active in international, collaborative networks to better understand multimorbidity and complexity, e.g. in the Multimorbidity Working Group of the European Federation of Internal Medicine or in a working group of the German Society of Internal Medicine on Artificial Intelligence in Internal Medicine.
The ICMC's innovation, science and support activities focus on the following objectives:
- Better representation of decision-making in complex situations
- Supporting decision makers at physician or systemic leadership level in the evolution of care for multimorbid patients or health system institutions
Projects
Hypertension/Cardiovascular Disease and Depression/Anxiety Disorders/Posttraumatic Stress Disorder (Ongoing):
Dana Blatch-Armon, Aliki Buhayer, Gunther Meinlschmidt, François Mach, Claudia Hackl-Zuccarella, Christian Appenzeller, Edouard Battegay
Depression and Generalized Anxiety Disorder or other forms of anxiety disorders are very prevalent in patients with cardiovascular disease (CVD). Quality of life and life expectancy worsen when these conditions co-occur. There are many disease-disease interactions, e.g. shortness of breath with coronary artery disease (CAD) and anxiety disorder that might be attributed to either condition that complicate patient management. Furthermore, therapeutic avenues may be narrowed by co-occurrence of disorders such as the question whether to use an antidepressant drug and if so which one. In a first study we evaluate how Clinical Practice Guidelines specifically address depression in patients with CVD, and whether they provide any operational guidance for screening and management of depression in the primary care and outpatient setting.
See the corresponding published protocol: https://pubmed.ncbi.nlm.nih.gov/37130663/
Total Hip Replacement and Depression/ Anxiety Disorders (Ongoing):
Martin Spoendlin, Edouard Battegay
This study aims to analyze the interaction between total hip replacement and depression, focusing on the predictors of readmission, patient behavior and postoperative outcomes. Using data from various studies, we will identify the key predictors, which significantly affect perioperative care, readmission and postoperative recovery. Hypothetically, by predicting postoperative outcomes and the need for targeted interventions through preoperative psychological screening, the recovery of patients with depression can be optimized and readmissions minimized, which may substantially improve the situation.
The occurrence of multiple diseases in the same patient (multimorbidity) often leads to problems due to incompatible processes. For example, patients taking an SSRI-type antidepressant tend to bleed more frequently during surgeries. Depression and anxiety disorders are common conditions, especially among patients suffering from chronic pain. Initially, scientific publications published between 2012 and 2022 that are thematically associated with preexisting depression and anxiety disorders and the outcomes of total hip and knee arthroplasty are to be identified. An initial search has found hundreds of publications (hits) addressing this topic. From these publications, those that examined these associations in detail will be selected and analyzed in detail. The results will be summarized in an appropriate form for orthopedic surgeons, nurses, physiotherapists, and other involved professionals to provide the best possible care and support for patients in considering depression and anxiety besides the orthopedic issues. Thus, we aim to gain and convey a deeper understanding of the topic of total hip and knee arthroplasty AND depression and anxiety disorders.
Lumbar Spinal Stenosis and Parkinson's Disease (Ongoing):
Peter Fuhr, Ute Gschwandtner, Edouard Battegay
The management of patients with lumbar spinal stenosis and Parkinson's disease presents unique challenges that are not adequately addressed by existing single-disease guidelines. Comorbid conditions frequently complicate both diagnosis and treatment strategies, necessitating comprehensive and integrated approache. This project aims to create clinical decision pathways that consider the interactions between diseases and medications, with a focus on operational guidance for healthcare providers.
Total Hip Replacement and Treated Parkinson’s Disease (Envisioned):
Please mail to edouard.battegay@multimorbidity.org, if you are interested in engaging in the project.
Parkinson's disease (PD) is a progressive neurodegenerative disorder that affects motor function and quality of life. Patients with PD who require elective surgery, such as total hip replacement (THR), are at increased risk for complications due to their underlying condition and the effects of anesthesia and analgesia. The purpose of studies on this specific issue is to evaluate potential disease-disease interactions in perioperative and postoperative care up to 12 weeks, and then potentially the possibilities of improved interdisciplinary care in the perioperative and postoperative period for patients with THR and treated PD.
Projects in Collaboration
Guideline-based clinical decision support framework for multimorbidity
Zijun Wang, Janne Estill and Yaolong Chen
Multimorbidity complicates the utilization of guidelines in clinical practice, since recommendations rarely consider comorbidities, and following recommendations from multiple guidelines may lead to overtreatment and be harmful. We aim to develop a guideline-based decision support framework for the management of multimorbid patients to help clinicians efficiently evaluate, select and adapt recommendations focusing on the different comorbidities and aspects of multimorbidity (see protocol at https://dx.doi.org/10.2196/preprints.63339). We are at present conducting questionnaire surveys and interviews among stakeholders and performing literature reviews to build an initial version of the framework. We expect to complete the framework within three years.
If you are a practicing clinician, nurse, or other healthcare worker who regularly or occasionally sees multimorbid patients, we would be grateful if you could participate in our online survey (https://www.surveymonkey.com/r/Y5H57J2) about guideline use. The survey takes only about 10 minutes to fill in, and details of the purpose are shown on the first page.
We welcome collaborations and are looking for partners e.g. to participate in our Delphi panel. If you are interested to contribute to this project, please contact the study coordinator Ms Zijun Wang (bdwzj_0312@163.com).
Impact for Clinicians